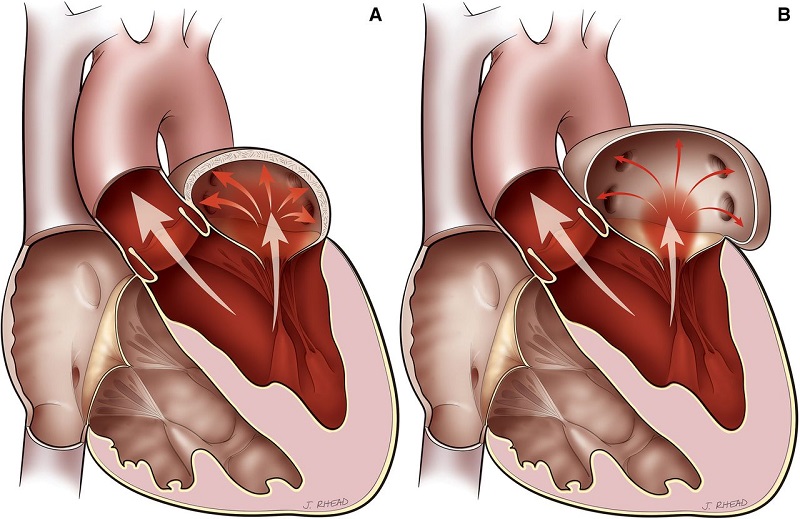
Mitral regurgitation (or mitral regurgitation) is a form of valvular heart disease, which is a disease of the heart valves, in which the mitral valve does not close properly when the heart pumps blood, causing abnormal backflow of blood in the opposite direction. the correct one (from the ventricle to the atrium).
It is the most common form of valvular heart disease and causes a systolic murmur (during the beating of the heart) that the doctor can hear through the stethoscope.
Often years pass before the defect becomes symptomatic because the extent of the expression depends both on the severity (how much blood flows back) and on the development time (a slow progression often allows the organism to gradually compensate for the difficulty, at least up to more advanced stages).
When present, symptoms include:
- Breathlessness and hunger for air,
- Easy fatigue,
- Palpitations,
- Swelling in the lower limbs.
Treatment of mitral insufficiency depends on the severity of the picture; If treatment is not usually needed in the early stages, heart surgery may be required to repair or replace the incontinent valve when regurgitation is severe.
Causes
The mitral valve separates the atrium and left ventricle, the side of the heart from which oxygenated blood is sent to the periphery through the aorta.
Its function is to hermetically separate the atrium and ventricle during the contraction phase, so that the pumping action is as efficient and effective as possible in expelling the blood outside the organ. In the event that the closure is imperfect, part of the oxygenated blood will tend to flow inversely, returning towards the atrium and this reduces the amount of blood that will be available in the periphery.
The possible causes of mitral regurgitation are numerous, but the most common are:
- Mitral valve prolapse and other valve defects
- Coronary heart disease and high blood pressure
- Infection of the heart valves ( endocarditis )
- Rare conditions, such as untreated syphilis or Marfan’s syndrome
- Rheumatic heart disease, is a complication of an untreated strep infection (expression of rheumatic fever )
- Hypertrophic cardiomyopathy
- Congenital heart defects
- Undesirable effects of chronic use of some anti-migraine medicines
- Chest radiation therapy exposure
- Atrial fibrillation
Mitral regurgitation can also occur suddenly, for example following myocardial infarction or chest trauma.
Symptoms
When the mitral valve imperfectly separates the left atrium and ventricle during the heartbeat, oxygenated blood may no longer be effectively pushed out of the organ due to regurgitation to the atrium. This could result in a lack of oxygen in the whole organism. If the regurgitation initially develops progressively, the patient does not manifest any symptoms thanks to the organism’s compensatory mechanisms, which can hide the pathology for years, however at a more advanced stage the following occur:
- Hunger for air, first under stress and gradually also at rest
- Breathing difficulty in a lying position
- Increased breathing rate ( tachypnea )
- Cough
- Easy fatigue
- Dizziness
- Palpitations and tachycardia
- Water retention in the legs
Complications
As oxygenated blood available to peripheral organs and tissues may be insufficient over time, the heart may attempt to compensate by pumping harder, however, over time this can lead to congestive heart failure, a condition in which the heart loses its capacity. to adequately supply the whole body with blood.
They can also develop:
- Atrial fibrillation, a dangerous alteration ( arrhythmia ) of the heartbeat that can expose the patient to thrombus formation,
- Pulmonary hypertension is a condition characterized by an increase in blood pressure in the pulmonary circulation, caused by the increase in pressure that progressively increases in the left atrium following reflux.
Diagnosis
The specialist doctor who deals with heart valve defects is the cardiologist, possibly the cardiac surgeon in case of need for surgery.
The first suggestive sign of the presence of mitral insufficiency is the characteristic murmur that the doctor is able to perceive by listening to the heartbeat; among the additional symptoms and signs useful to form suspicion during the visit are found
- Edema of the lower limbs (localized swelling of the legs and ankles)
- Liver enlargement
- Enlargement of the neck veins.
Among the tests useful for the diagnosis and the complete classification of the condition are:
- Echocardiogram, the examination of choice, which allows the study of the structure and functionality of the heart through the use of harmless ultrasounds;
- Electrocardiogram , useful for the electrical study of the heart (mitral insufficiency progressively causes the development of changes in the beat),
- Chest x-ray, which may show pathological enlargement of the left atrium/ventricle,
- Mri and ct scans, finer imaging tests than x-rays,
- Exams under stress, are useful to define the seriousness of the picture.
Treatment
The course and prognosis of mitral insufficiency are widely variable, in relation to the causes and general health of the patient.
Most of the time the condition is mild, so much so that it does not require any therapy or restrictions, beyond regular check-ups (watchful waiting).
Symptoms, when present, can be controlled by drugs and obviously a correct treatment of any pathology responsible for the onset of the valve defect is essential (for example, high blood pressure must be treated). Among the medicines most used for this purpose are
- Beta-blockers, ace inhibitors, calcium channel blockers,
- Anticoagulants,
- Antiarrhythmics,
- Diuretics.
In more serious cases, surgical repair/replacement of the mitral valve may be required, especially if:
- The heart function is no longer able to guarantee an adequate supply to the organism
- The heart is severely dilated
- The symptoms worsen and are no longer pharmacologically controllable.
Lifestyle
Lifestyle improvement can significantly influence the evolution of the disease, especially when the diagnosis occurs in the early stages; patients with mitral regurgitation are generally advised to
- Stop smoking
- Lose weight if necessary
- Adopt a varied, healthy diet rich in fruit and vegetables (such as the Mediterranean model) and low in salt (such as the DASH diet )
- Reduce or abolish the consumption of alcohol
- Practice regular physical activity